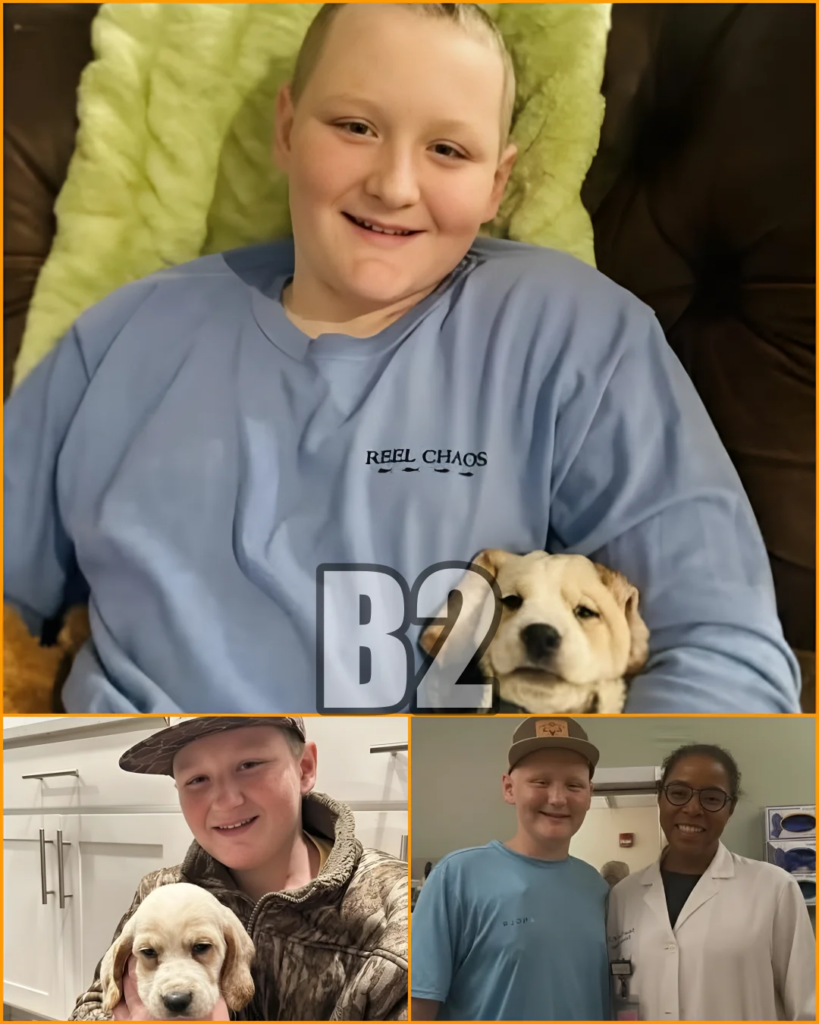
TST. After days of holding their breath, the Roberts family is finally able to exhale.
Exhaling at Last: Why Will Roberts’ Latest Scan Brought Relief — and What It Really Means
For forty-eight hours, time moved differently for the Roberts family. Every hour felt heavier than the last as 14-year-old Will Roberts underwent extensive imaging at Children’s of Alabama. Scans are never just scans in pediatric oncology; they are verdicts-in-waiting, moments that can redraw the emotional map of an entire family’s life. When the initial report arrived, confusion followed. But what came next changed the emotional trajectory of the week — and, for now, the outlook of Will’s fight.
An addendum to Will’s PET scan clarified the picture, and with it came a cautious but genuine sense of relief. According to his mother, Brittney, the updated interpretation showed that most of Will’s cancer sites demonstrated lower uptake than before. In medical imaging, those words matter. They do not suggest cure, nor do they close the chapter. But they do indicate something profoundly important: the treatment is doing what it is supposed to do.
To understand why this matters, it helps to understand what PET scans actually measure. A PET scan doesn’t simply show where cancer exists; it shows how active it is. Areas of high uptake signal aggressive metabolic activity — cancer cells burning energy rapidly. Lower uptake means those areas are quieter, less active, less aggressive. In plain language, the disease is cooling down rather than flaring up.
That distinction is the difference between escalation and stabilization — sometimes even improvement.
In Will’s case, the addendum made clear that the findings did not represent widespread progression. That phrase alone lifted an enormous weight. For families walking this road, progression is the word everyone fears most. It signals not just medical change, but emotional upheaval: new decisions, new risks, new uncertainties. What Will’s scans showed instead was a trend pointing in the opposite direction.
Brittney did what many parents now do when faced with dense medical language: she turned to AI to help translate the jargon into something human. The simplified explanation confirmed what her instincts already sensed. The scans told a story of response, not retreat. Of effort being met with effect.
That moment — when a parent’s intuition aligns with medical evidence — is powerful. It doesn’t erase fear, but it steadies it.
Importantly, this update does not mark an endpoint. Pediatric oncology is rarely linear. Improvement in one scan does not guarantee smooth sailing ahead, and no responsible doctor would frame it that way. That is why Will’s oncology team will meet again on Monday, carefully reviewing the data and determining next steps. Medicine moves forward one decision at a time, especially when the patient is a child.
But milestones matter. And this one matters deeply.
In the world of childhood cancer, victories are often quiet and incremental. They don’t always look like ringing bells or declaring remission. Sometimes, a victory is simply hearing that things are not getting worse — that the ground beneath your feet is holding. Sometimes it’s learning that the medicine is reaching its target. Sometimes it’s being told, “This is not what we feared.”
Those moments deserve to be honored.
What makes Will’s story resonate so widely is not only the medical update, but the emotional honesty surrounding it. Brittney did not present the news as triumphal or definitive. She acknowledged the anxiety, the confusion, and the fragile nature of hope in situations like this. That balance — between faith and realism — is what families facing serious illness recognize instantly as authentic.
The response from the broader community has reflected that recognition. Messages of prayer, encouragement, and solidarity poured in not because the fight is over, but because people understand what this moment represents: breathing room. A pause in the storm. A reason to gather strength for the next stretch of the journey.
For Will himself, a 14-year-old navigating a world no teenager should have to know, the implications are deeply human. Fewer aggressive cancer signals mean more energy preserved, more resilience protected, more space for his body to keep fighting. Even small physiological improvements can translate into meaningful differences in how a young patient feels day to day.
This is why oncologists pay such close attention to trends, not just snapshots. Cancer treatment is about momentum as much as milestones. Right now, the momentum is not moving in the wrong direction — and that matters enormously.
The phrase “keep the prayers coming” is sometimes dismissed as ritual language. But in moments like this, it functions as something else entirely: a recognition that no one walks this road alone. Prayer, support, shared attention — these are not substitutes for medicine, but they are companions to it. They sustain families through the waiting, which is often the hardest part.
Will’s journey is not finished. No one is pretending otherwise. But today, there is room to exhale. To acknowledge progress without tempting fate. To celebrate effort without declaring victory. To hold hope carefully, but firmly.
In pediatric cancer stories, there are chapters marked by heartbreak and chapters marked by resilience. This update belongs to the latter. It does not promise the ending — but it strengthens the middle.
